Menu


Getting Started Fishing
Amanda Olsen
April 19, 2024

Double Emergence: Cicadas Taking Over Midwest
Amanda Olsen
April 12, 2024

Sloth Saga Enters New Phase
Cole McDonnell
April 5, 2024

Officials Unite Against State Housing Plan
Amanda Olsen
April 23, 2024

Children’s Service Providers Get Crucial Pay Bump
Anton Media Group Staff
April 23, 2024
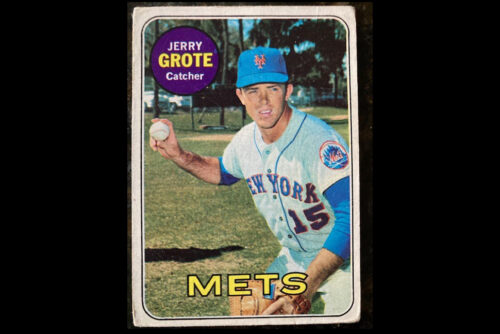
Fond Memories Of Jerry Grote
Amanda Olsen
April 22, 2024

Opponents Of ‘Blakeman’s Militia’ Rally In Mineola
Janet Burns
April 12, 2024

Attacking Our Courts Undermines America
Jerry Kremer
April 22, 2024

Can The MTA Manage $15 Billion Carryover Capital Projects With The Next $51 Billion Or More
Larry Penner
April 15, 2024

Shine A Light For Charity On The INN
Kayla Donnenfeld
April 15, 2024

The Big Move
Marisa Cohen
April 15, 2024
LOCAL EDITIONS
TRENDING
(Photo from NBCUniversal)
Chuck Scarborough:
A Beacon of Journalistic
Longevity
By Christy Hinko • April 22, 2024
THIS WEEK'S
SPECIAL SECTIONS